My name is Jamie Childs Everett and I am the current president of the Wyoming Physical Therapy Association. Firstly, thank you for allowing me to speak on Wednesday, August 29th during the public forum and I apologize if the following is more than needed at this time. I will preface my following statements as they will be more geared towards non-opioid solutions as my knowledge base is with physical therapy and will always endorse this as a first option in cases where I feel that physical therapy is appropriate and sometimes overlooked. However, I am fully knowledgeable that physical therapy is not always the best option and, in some cases, such as
What I know the most is that pain is confusing. I can’t even tackle the thought of understanding what, when, and how to educate on prescribing opioids. But what I do know is that there is a void on interdisciplinary communication and education on pain management for all healthcare providers, including the allied health professionals and mental health providers. The Institute of Medicine on their report Relieving pain in America 2011 argues that economic and human tolls have been created by the ineffective treatment of chronic pain in our current health care system. The following is an attempt to convey thoughts regarding this, so I apologize if there seem to be missing points, but I will happily provide any resources including articles that will fulfill any questions. I have left out other discrepancies in health care such as poor reimbursement, high cost of copays, and patient access to non-pharmacological treatments, but would share as well if requested.
I spoke briefly suggesting the current bill endorse a broader topic of standardized multifaceted pain management education across all the health professions while remaining inclusive of opioid education to those who prescribe it. In brief, we give myopic attention when our medical management causes related deaths, but the current epidemic is not just about opioid addiction and its associated problems; it is a pain management problem. I hope you find the time to read the following as I elaborate my basis for this statement.
It is fair to say that every health care provider sees patients with pain. Creating a bill that only educates those who prescribe opioids leaves a potential void to other healthcare providers and the patients they treat. Without a consistent message throughout the health professions that is integrated into a multidisciplinary education model that specifically provides information on pain and non-pharmacological pain management solutions, Wyoming providers could fail to discuss or offer non-opioid options that address patients’ needs. Potentially leading a patient to the understanding that only imaging, opioids, or surgical intervention is the answer to reducing their pain, when there may be other options. Currently for chronic pain the CDC recommends nonpharmaceutical approaches such as physical therapy over opioids. (Dowell et al 2016). A study in 2003 by Mosely et al communicated that health care providers may have poor knowledge of current information about pain and cannot clearly communicate to patients why they hurt. Communication should educate the patient that pain is an output of the brains perception of tissue danger which can be interpreted based on biopsychosocial factors rather than specific tissue damage. Louw et al 2016 provided evidence that education about biology of pain may reduce pain and disability and improve function and movement compared to those who did not receive the education prior to surgical interventions.
Just to continue with more evidence of this need for collaborative education stands with the fact that people who have pain visit healthcare providers with a desire for more information because they trust healthcare providers. Because of this trust providers are in a strong position of influence. The information received from the provider can influence in a positive or a negative manner about the patient’s perception of their pain, which can lead to the need for more opioid based medication or in contrast the understanding of assuming a more active lifestyle. What can lead to more anxiety and fear of pain is when the message is delivered in a biomedical language from providers, for example being told that you have degenerative disk disease or disk bulging can lead to catastrophizing, lifelong disability and thoughts of eventual paralysis. In contrast to getting told you have normal aging in your spine with the facts that there are many people asymptomatic with evidence of bulging can shift patient focus to recovery and empowerment to reduce fear. This change of language is just a condensed version of what standardized pain management would encompass. (Stewart et al 2018)
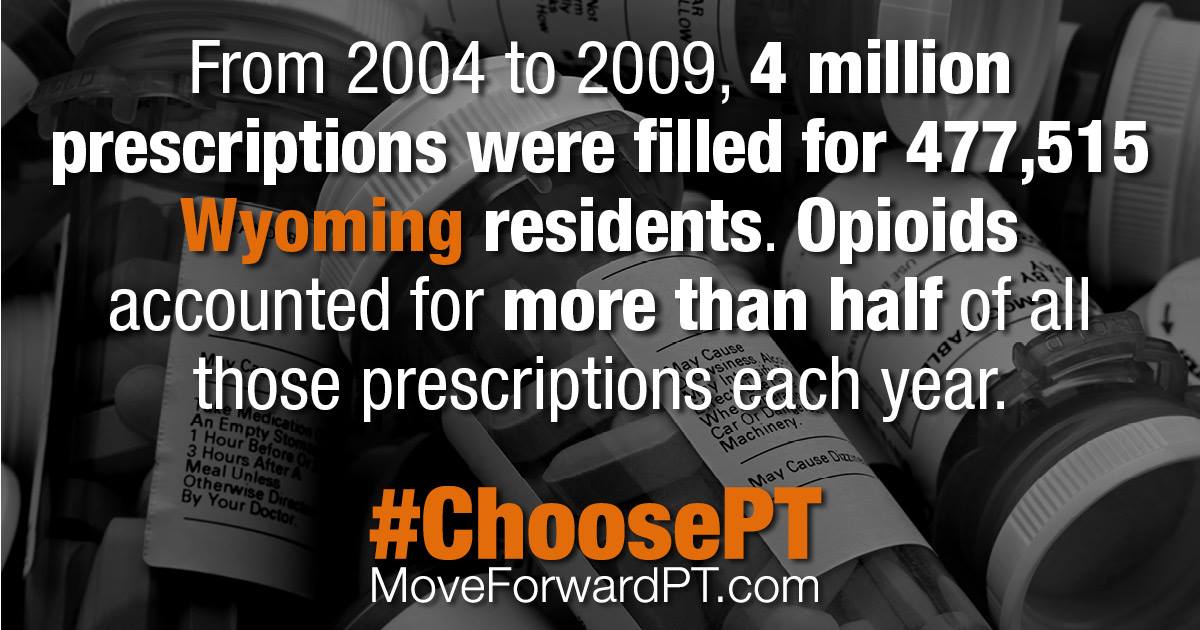
It is alarming to think that because of the ease to prescribe, ease to obtain, and ease of coverage from insurance coverage that opioids or other pharmacological interventions are the first choice for pain management. This thought seems contrary to a recent Gallup poll in 2017 finding that indicates 78% of Americans would prefer to address physical pain by other methods rather then take pain medication as prescribed by their physician.

A published report in 2017 by Zheng et al (authored by MDs) in the Spine Journal states a lack of education to the public about alternatives to pain management has most likely resulted in a rise of opioid prescriptions and the stagnation of alternative options for low back pain such as physical therapy. The authors concluded that “despite…Physical therapists promoted as a first-line treatment for low back pain, (physical therapy) referral rates remain low. There also exist disparately lower referral rates in populations with restrictive health plans and simultaneous opioid prescription…(this) isolates concerning associations requiring further explorations. The continued low rates of physical therapy referrals for patients with low back pain suggest that initiatives are needed to educate both providers and patients about the utility of physical therapy” This report proceeds the recent American College of Physicians most current clinical practice guidelines in 2017 on acute to chronic low back pain which recommend nonpharmacologic treatment approaches such as physical therapy that include spinal manipulation, exercise, education on behavioral changes, and recommendations to stay active.
Another reason to shrink the knowledge gap and pursue unified pain management education is verified in the published study in 2015 from Lev et al in the American Journal of Emergency Medicine revealing that the specialty of primary care comprised 54% of the prescriptions that resulted in substance abuse followed by emergency medicine at 20%, psychiatry 11% surgery 8% dentistry 4% and pain 3%. Another study by Thackeray et al reported that referral to physical therapy and participation with physical therapy were associated with reduced opioid prescriptions. And lastly, a study by Childs et al in 2015 showed that early access to physical therapy reduced opioid use by 62%, decreased imaging by 56% and had better outcomes.
I am not aware that anyone has really come up with the best strategy or a simple answer for dealing with pain, but if Wyoming health providers can integrate a team approach for patient care and approach pain management with standardized, informative, and simplistic pain management maybe we can get one step closer to a best strategy supported by best practices. The more voices that educate about pain in the same manner the louder the message will become to the public regarding options for pain management other than opioids.
These proposed educational mandates given across all spans of Wyoming healthcare providers can give patients unified information about options for pain management. Training and educational resources directed to both opioid prescribers and other health care providers in Wyoming should convey the value of nonpharmacological treatments and how to recognize when there are safer and more effective options for the individual’s condition.
I understand that mandating specific regulations onto multiple boards is a dauting task, but the incentive is for standardizing best patient care approach in Wyoming. To dictate a comprehensive pain management bill could without a doubt take years to define and education would take hours to complete, so I propose a simplistic outline from knowledgeable professionals collaboratively instructing on pain and pain management.
The pain education proposed could be provided by several Wyoming healthcare providers on a cooperative front including but not limited to basic education on fundamentals of pain, neurophysiology of pain, the pain neuromatrix in comparison to the Cartesian model of pain, how pain can be perceived or experienced based on several personal and cultural factors and beliefs (mature organism model), collaborative language to be used to the patient, education on function with lessening focus on the fifth vital (pain), beliefs about pain and disability, therapeutic alliance with patient and clinician, chronic pain alterations of brain, opioid induced hyperalgesia and allodynia, pharmacological treatment, multifaceted approach with tapering from opioids, non-pharmacological therapies including but not limited to physical therapy, and benefits of exercise to produce naturally occurring endogenous opioids.
At one time on Wednesday during the Task Force meeting, I heard mentioned that healthcare providers need to be aware of non-opioid alternatives, but these suggestive alternatives were of other medications not about alternatives such as physical therapy, mental health counseling, massage, meditation or any other healthcare providers. The Wyoming Physical Therapy Association currently is trying to standardize pain rehabilitation education amongst our membership by bringing in experts from around the country to instruct our membership. But we have come to the realization that this need is much bigger than just our profession and needs to be expanded. The broader purpose of proposing pain management education to all healthcare providers would establish a common language and background amongst our health care providers in the state of Wyoming.
A report by the New York Times indicated that Wyoming is one of the leaders in the country by demonstrating a decrease of
Thank you for your time
Jamie Childs Everett, PT, DPT, OCS, FAAOMPT
Wyoming Physical Therapy Association President
307.421.4094
Research and articles referenced: (additional research available upon request)
Americans prefer drug-free pain management over opioids. Available at: http://news.gallup.com/reports/218495/s.aspx?utm_source=link_newsv9&utm_campaign=item_217676&utm_ medium=copy. Accessed December 31, 2017.
Childs, JD., et al. “Implications of early and guideline adherent physical therapy for low back pain on utilization and costs.” BMC health services research 15.1 (2015): 150.
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA. 2016;315:1624-1645. https:// doi.org/10.1001/jama.2016.1464
Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011.
Lev R, Lee O, Petro S, et al. Who is prescribing controlled medications to patients who die of prescription drug abuse? Am J Emerg Med. 2016;34:30-35. http://dx.doi.org/10.1016/j. ajem.2015.09.003
Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. 2016;32:332- 355.
Moseley L. Unraveling the barriers to reconceptualization of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain. 2003;4:184-189. https://doi.org/10.1016/ S1526-5900(03)00488-7
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514-530. https://doi.org/10.7326/ M16-2367
Stewart, Michael, and Stephen Loftus. “Sticks and Stones: The Impact of Language in Musculoskeletal Rehabilitation.” journal of orthopaedic & sports physical therapy 48.7 (2018): 519-522.
Thackeray A, Hess R, Dorius J, Brodke D, Fritz J. Relationship of opioid prescriptions to physical therapy referral and participation for Medicaid patients with new-onset low back pain. J Am Board Fam Med. 2017;30:784-794. https://doi. org/10.3122/jabfm.2017.06.170064
Zheng, Patricia, et al. “Stagnant physical therapy referral rates alongside rising opioid prescription rates in patients with low back pain in the United States 1997–2010.” Spine 42.9 (2017): 670-674.